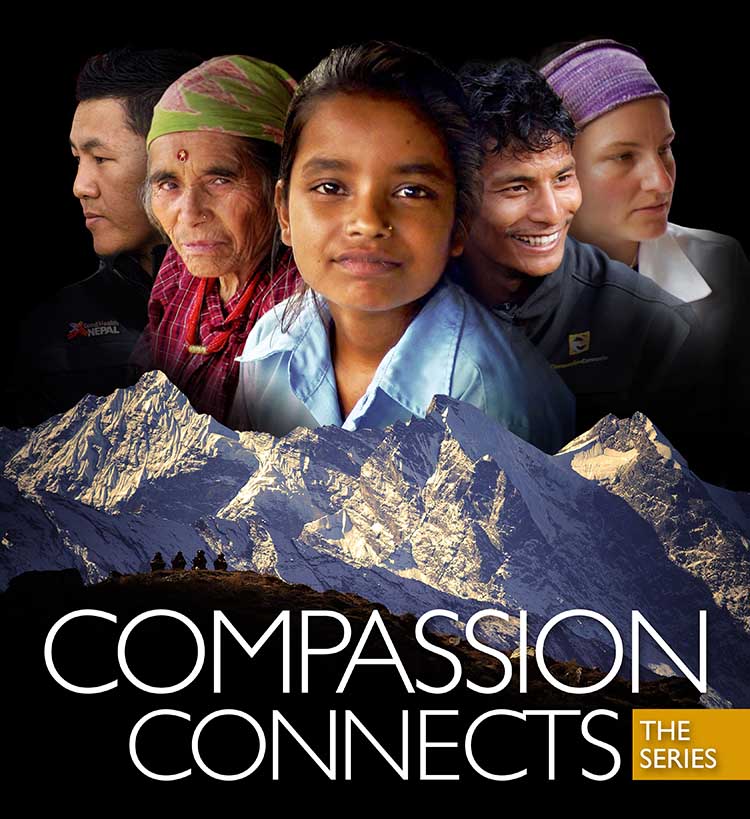
Documentary filmmaker Tristan Stoch returns to Nepal in 2015 to follow up on his 2012 work Compassion Connects. This new series of seven short films focus on Acupuncture Relief Project’s current work in rural Makawanpur Nepal.
During our premiere screening in Portland Oregon, several guest speakers shared personal stories about their experience in Nepal. Some of these stories have been shared here. Please Enjoy.
Episode 1: Rural Primary Care
In the aftermath of the 2015 Gorkha Earthquake, Andrew Schlabach, Director of the Acupuncture Relief Project and Tsering Sherpa, Director of Good Health Nepal begin a new primary care clinic in the rural district of Makawanpur. This episode explores the challenges of providing basic medical access for people living in rural areas.

Sheri Barrows: Why Acupuncture?
Board of Directors, Secretary/Treasurer, Acupuncture Relief Project
Participating on the Board of Directors since ARP's inception, Sheri was able to spend the 2015/16 season in Nepal with the clinic teams. Seeing first hand the complexity of practicing medicine in rural villages she came home with a better understanding of the challenges in accomplishing our mission.
This last year I was extremely fortunate to have taken a long hiatus from my paying work so that I could be in Nepal to help get the new clinic set up and to witness first hand how things were going in both Bajrabarahi and Bhimphedi. I had a hard time deciding what I was going to talk about tonight because there were so many stories to choose from but I kept coming back to one story that really moved me.
I was in the Bhimphedi clinic, standing near the door and I looked outside and watched a man being helped through the gate by about 4 people. He needed the support of all of them because he had had a stroke and the left side of his body was severely paralyzed. When it was his turn, he was brought into the clinic and Rachel Hemblade from the UK became his doctor. We learned through his wife that his name was Jagat and the stroked had happened about a year before. He was completely unable to speak and vocal testing showed that he could only achieve a barely audible sound for one vowel.
The thing that broke my heart with Jagat was how completely and utterly dejected he was. He had gone from being a 35 year old husband and father of three kids and a valuable community member to being totally dependent on others.
I have never in my life met someone as completely hopeless as Jagat was on that first visit.
Rachel told Jagat’s wife that for the best results he should come to the clinic every day for at least a few weeks and she asked if that would be possible. They live up in Bhimphedi 3, which is about a 4 hour walk from the clinic, but they were able to make arrangements to stay with family that lived just down the road. Rachel then enlisted the help of all of the family members that were at the clinic with him that day, including one of his young sons. She showed them some physical therapy exercises and she showed them how to help him form the sounds of the English vowels and told them they should practice all of it twice a day. When Jagat came to the clinic the next day I greeted him near the gate and though he wasn’t able to show hardly any facial expression I saw a faint sparkle in his eyes that hadn’t been there the previous day. By the end of that second treatment Jagat was able to make the sounds of all the vowels and he had regained a slight amount of movement in his left foot and hand so that when he left the clinic he was able to use a cane in his right hand and just one person supporting him on the left. As he passed me going toward the door I was so thrilled by his improvement that I gave him a little cheer and this time when he looked me in the eye there was a strong sparkle and a slight twitch at the corner of his mouth as he tried to smile.
Between the Acupuncture, Massage from Sarah and the homework he so diligently did, Jagat improved very quickly and by the end of the first week he no longer needed his wife to speak for him and was able to answer all of Rachel’s question himself, albeit slowly, and the muscles in his face were able to form a smile that lit up the clinic. Also by the end of that first week he was walking to the clinic by himself with just the aide of his cane and by the end of the third week he was able to stop using the cane all together.
After a month or so Jagat went back home to Bhimphedi 3 and would make the 4 hour walk to the clinic a few times a week for treatment. His doctor during Camp B told me that by the time she left in December, he had recovered about 70-80% of the abilities he lost to the stroke.
This story of Jagat is just one of so many examples of how the clinics make a difference and change peoples lives and I cannot begin to tell you how meaningful it has been for me to have been there and experience it for myself.
Episode 2: Integrated Medicine
Tackling complicated medical cases through accurate assessment and the cooperation of both governmental and non-governmental agencies, Acupuncture Relief Project extends the reach and effectiveness of it's medical model. This episode follows the stories of two patients who's care required a coordinated effort.

Sarah Richards: Heart
Acupuncture Relief Project Volunteer 2012, Team Leader 2015
Sarah has been a body worker since 2000 and has been to Nepal twice with ARP. She has recently stepped into the role of Volunteer Coordinator as a way to continue service to the project and to help support practitioners endeavoring to bring their healing arts to the people of Nepal.
I'd like you to bring your memory to the beginning of this last segment, To the story of the woman Hira Maya who had a life saving diagnosis that led her to heart surgery one year before this interview took place.
I had the honor and the extreme privilege to be there last year and treat her. I already knew of her interesting case based on the blog written about her the prior year and was eager to see her and hear how she was doing.
When she first came in, this is what I observed:
small, slight, tiny and yet heavy and weighted
pale
quiet
withdrawn
shy, timid
under-nourished
very shallow and labored breath
hesitant
I say hesitant because she was not sure she wanted to receive any Tx, she thought we just wanted to do the interview and so she wasn't expecting, or maybe even wanting Tx. But with a little coaxing she agreed to let us take vitals and to get on the Tx table for a little body work.
I don't have enough time to go over all the details, but after 3-4 short Txs to address the major rib cage trauma and scar tissue from having heart surgery a third world country, here is what I observed:
bright
talkative
colorful
smiling
making eye contact
willing and eager to receive treatment
and most importantly to me, she was breathing deeply and with ease
I know this change sounds dramatic, but it truly was....and it left a searing impression on me. Very little Tx resulted in dramatic change. Her presence, her essence was palpable from across the room, where before it was diminished.
Now, it is my belief, based on my experiences in Nepal, that it was not only the Tx but also the nature of the clinic itself that created this change in HM. The fact the Hira Maya had a place to go where health care workers were deeply concerned with her well being lifted a heavy weight off her chest.
The ARP clinics are a gathering place for community, a hive where healers and patients come together with curiosity and compassion, where deep listening occurs, where gentle touch is applied and where cultures collide to create a vortex of possibility.
My favorite part about the ARP experience is that the clinics in Nepal provide a testing ground for practitioners to to see what really matters in medicine. It affords a concentrated experience where your skills get stripped down and your fears highlighted to illuminate your greatest strengths and also your weaknesses. Maybe it's needles, herbs, touch, attitude, stamina, technical knowledge, intuition, presence, empathy or compassion, it all gets tested.
This sort of experience paves the way to build the foundation of understanding who we are as healers. Or like the phoenix, in some cases the experience burns and destroys only to then re-birth and re-build, this is where authentic healing and wisdom unfolds, for patients and practitioners alike.
Hira Maya gave a me a precious gift, thru her trust in me, she illustrated in a very vibrant way that when a clients case seems extreme, that when I'm not sure I have the skills to ease their suffering, when I ask myself how can a simple massage soothe something so complicated,
here comes the gift.....
presence, willingness, deeply listening and taking action from the heart, and rooted in compassionate loving kindness IS enough! I AM enough!
And it is with the strength of this knowledge I honor Hira Maya and bow to her in deep gratitude for this teaching and healing!
There is more to this story, yet my time with you is short, keep an eye on the ARP blog for updates and more stories like this.
Because I have valued my experience greatly with ARP I am developing the role of Volunteer Coordinator as way to continue my service to the project and support practitioners on their journey of growth, if you find yourself inspired by this event tonight, please reach out, volunteering is the biggest donation that we can receive!
Episode 3: Working with the Government
Cooperation with the local government yields unique opportunities to serve the rural population. Acupuncture Relief Project is invited to help establish a new integrated medicine outpost in Bajra Barahi, Makawanpur, Nepal. This exciting prospect enables ARP to forge a new clinic model applicable throughout Nepal.

Diane Wintzer: Primary Care
Project Coordinator, Acupuncture Relief Project Volunteer 2008, Team Leader 2010, 2012
A graduate of Oregon College of Oriental Medicine, Diane runs a very busy practice in Camas, Washington. Drawing upon her experience with Outward Bound she has helped Acupuncture Relief Project develop their training and mentorship programs.
About 9 months ago, I received a call from a senior patient whom I usually treat twice a month. She had a special request that day. She was wondering If I could rub some good smelling oils on her that would help her breath easier. According to my patient, her primary care doctor had just diagnosed her with bronchitis for the 3rd time this summer, and she was really having a hard time breathing. She was very difficult to hear over the phone, and I weighed out my desire to see what was going on against how much energy it would take her to get to the office. I knew it was a hot day, it was a 30 minute drive for her, and the passenger seat in her car didn’t recline which was hard on her back. I told her I’d like to see her, and that I had some things we could do to see if it would improve her breathing.
A few hours later my patient arrived. I noticed her ashen skin tone, her weakened voice, and her off-balance shuffle as we walked to the treatment room. But the check in was business as usual. I asked questions about her most recent visits to her PCP, her blood sugar numbers, and what she was getting done around the house. She reported a recent fall that left some bruising on her legs, but could not really say why it happened - she didn’t trip - she just sort of tumbled. She had been to a “fill-in” PCP (not her usually doctor) 2 days prior for her coughing and breathing difficulty, and after some assessment, he prescribed cough syrup with codeine and told her to get some better rest, and he provided antibiotics. In truth, my patient wasn’t sure if the doctor told her she had bronchitis or pneumonia.
She continued to share. She’d been sleeping in the recliner for a few nights because it made her feel better. She hadn't felt much like eating or getting outside. I noticed my patients short sentences, the time it took her to share, again the quiet voice, and her lack of clarity around things. She got onto the treatment table, and as I examined her bruising, I noted that it did not match up to the story all that well. She had fallen hard, and due to blood thinners, she was severely bruised from her ribs to her knees. I noticed my patient minimizing her injuries. I noticed her anxiety increasing rapidly while laying back on two pillows. I switched gears, sat her up in a chair, put some ear needles in to calm the anxiety, and began to compile the list of symptoms: Extreme shortness of breath; Leaning forward to naturally make breathing easier: Elevating her shoulders to use accessory muscles for breathing; Severe pitting edema in the lower legs that was not normal for her; The gray color to the skin; The confusion around details when she is usually sharp as a tack and full of story. I tried to take a blood pressure reading… it was barely readable.
I looked at my patient and without wanting to freak her out, simply stated that it was time to call an ambulance and go to the hospital because she was in cardiac distress. She had enough in her to argue me just a bit, just enough spirit to reach for the bronchitis diagnosis and being run down, just enough to tell me of the retirement party she was going to after this appointment of an old co-worker, and that the ambulance was too much money. I wrote out the base line symptoms quickly on paper and slid them in front of her so she could see them, and reminded her she was not going to be able to compensate for very long.
To make a long story short, my patient ended up with a diagnosis of acute Congestive Heart Failure, and had a week long stay in the hospital. A few weeks later the doctors managed a heart surgery where they repaired some failing valves. Just last week, after 9 months, she felt strong enough to come back in for acupuncture treatment. Recovery was hard as she, in the end, realized that she had been declining for a while, and just missed it. Today though, she was sharp as a tack, full of stories, and back to her household projects. And of course, she wanted some good smelling oils rubbed on her back.
Most days, this is not the case. Emergencies do not walk in the door frequently. People come in with sore backs, sore knees, insomnia, stress, digestive distress, fertility help, constipation… you name it, but some days the story someone tells has some anomaly in it, some aberration that stands out, or I just get some intuitive hit that something is not lining up. The more stories, the more patient touches, the more willingness to engage my patients, the more I find my idea of medicine being stretched. I am grateful to ARP for nurturing my ambitious heart and curious mind and expanding my ideas of what it means to be practicing acupuncture. I had no idea that being the best acupuncturist I knew how to be, would be a moving target, and would include days where my needles never came out of the package.
Episode 4: Case Management
Complicated medical cases require extraordinary effort on the part of Acupuncture Relief Project staff and volunteers. Illiteracy and the inaccessibility of medical facilities are major obstacles requiring innovative case management. This episode follows 4-year-old Sushmita in her battle with tuberculosis.

Terry Atchley: A long way from help
Acupuncturist, Acupuncture Relief Project Volunteer 2013, Team Leader 2015
A native of New Orleans and graduate of the Oregon College of Oriental Medicine, Terry traveled to Nepal to help open a new primary care clinic in Kogate. This experience allowed Terry to treat a multitude of illnesses and develop her connection to people through words, touch and understanding.
“Grief can be the garden of compassion. If you keep your heart open through everything, your pain can become your greatest ally in your life's search for love and wisdom.” Rumi
At 2am on my last night in Kogate I woke to someone pounding on the door. As the only medical team in this remote region we were sometimes called for emergencies. The patient was a young pregnant woman with pain and bleeding. I got dressed and hiked the steep trail to her house. As I entered her home, I saw the young woman was scared. She looked at me for reassurance and safety. I spoke with her and learned she was seven months pregnant and had a history of late term miscarriages, one which occurred when she was alone in a field.
I checked her vitals and listened for a fetal heartbeat, but heard silence. At this time I believed she was having a miscarriage and began to explore my options. I called for a rusty old land cruiser that functioned as an ambulance to take her to the nearest hospital which was two hours away down a very rugged terrain. I tried my best to comfort her as we waited. I felt helpless and incompetent. There was nothing I could do, but bear witness, hold her hand and offer comfort.
The dusty vehicle arrived with a single driver, it had a lengthwise seat in back with a spare tire on the floor and an ancient oxygen tank. I was not able to travel to the hospital with her and would not be able to follow-up with her after she got there.
The next day, as we were leaving Kogate, I received an update. She had given birth to a stillborn on the way to the hospital.
I think of this patient almost daily. When I returned to Nepal in 2014, I was eager to see her. I wanted to tell her all the things I couldn't say in the moment. Sadly, I learned she no longer lived in the village. She had divorced her husband and returned to her parents house in India.
This experience broke my heart. But this heartbreak helped me learn what it truly means to be a healer.
I had to look beyond objective findings, results or a cure. I believe being an excellent healer means sometimes we have to let go of the outcome. I had to let go of the notion that I needed to solve every problem to be validated as a practitioner. The answer to this case was not found in all the intellectual learning from school, but in my heart. I gave the only thing I could give in the moment- compassion. I had to release the expectation I had of myself as a practitioner and accept that my ability to care for a patient sometimes has nothing to do with medicine and everything to do with love.
Episode 5: Sober Recovery
Drug and alcohol abuse is a constant issue in both rural and urban areas of Nepal. Local customs and few treatment facilities prove difficult obstacles. Partnering with Sober Recovery, one of the few inpatient acute detox rehabilitation facilities in Nepal, Andrew Schlabach and Tsering Sherpa train volunteers in the use of acupuncture.
Episode 6: The Interpreters
Interpreters help make a critical connection between patients and practitioners. Recruiting local young men and women, Acupuncture Relief Project provides a unique training and employment opportunity. This episode explores the people that make our medicine possible and what it takes to learn job.

Bex Goebner: Death and Dying
Acupuncturist, Acupuncture Relief Project Volunteer 2015, Team Leader 2017
Bex lives in Northeast Portland with her partner and two young boys. In 2015, she visited Nepal and found some of the most meaningful teachers of her life in the patients she treated there. She is forever grateful for the mind-blowing, heart-opening experience that ARP has offered to her.
Lal Bahadur Lama had been an entertainer and artist for most of his life, though at the time I met him, he was a farmer. He grew up in Kathmandu, where he was trained as a painter and sculptor. In his early years, he would leap the steps of the Monkey Temple and position himself on a ledge. From there he would draw the snowy shadows of the Himal.
After he married Vagawoti Lama and took up residence in the village, he became part of an entertainment troupe. His beautiful wife would smile when she attended his stage shows for the King and Queen in their summer palace. On one of his favorite nights, Lal and his nephew wheeled out a life-sized elephant he had built and painted. As he stood in front of the king, Lal flipped a switch and the elephant’s spring-loaded trunk swung up in a posture of salute while the crowd cheered.
As a farmer, he missed his artwork, so he took up a side job with the Nepalese forestry department, where he could wander around taking photos. He decided to use some of this work to open up a photo shop in the village. He quickly put himself out of business by giving all his inventory away to his friends. He was bummed about this failure but proud of his generosity.
In 2015, I arrived in the village of Bhimphedi to find this 71-year old man. The clinic hadn’t opened yet but I got a call to his house for a respiratory emergency. I’m still not quite sure how it happened, but I was able to get him stabilized. ARP doesn’t typically do home visits, but I began going to see him most nights of the week.
Usually after dinner, I would visit his cold room to listen to his lungs and check his oxygen levels. I would hear his heart beat and notice that the second sound lingered too long. I would press into his right foot to make a deep pit and count the minutes until it refilled. I'd take a look at the rusted welding tank that fed him, making sure that his family hadn’t turned it down to save money. After I did this, I would sit next to him and hold his left hand, the one that wasn’t swollen. When he could catch his breath, he’d tell me who he had been.
Lal was dying from the end stages of emphysema, though he’d never smoked a day in his life. The honeycomb cysts in his lungs came from growing up in a Nepalese home with an indoor cooking fire. It was worsened by walking the polluted streets of Kathmandu, where the brick industry blackens the air.
Thirty times after I visited Lal, he died in the middle of the night. All of the funerals I had seen in Nepal were Hindi funerals. The dead were taken to the rivers, covered in marigold flowers and burned. Lal was put into a simple white coffin painted with a thick red cross. He was lowered into a deep hole in the dried riverbed and his flowered bedspread was folded on top.I kneeled there while the women wailed and people threw handfuls of dirt and roses into the hole.
In the end, we share the best memories we have and these memories go beyond where we live or the clothing we wear. It doesn’t matter whether we are the dying person or the witness in the room. At that moment, we cannot help but be united in our humanity.
Episode 7: Future Doctors of Nepal
Acupuncture Relief Project begins the process of training and licensing local practitioners. This critical step towards sustainability requires partnership with other organizations as well as the national government. This episode looks at the people and the process of creating a new generation of Nepali rural health providers.