Allissa Keane RAc
November 2013
OVERVIEW
38-year-old female presents with a 4-year history of involuntary spasming throughout her entire body. The patient does not have any available medical records and the cause of spasming is unknown. Over the course of treatments, the patient experienced a feeling of ‘lightness’ in her body, especially immediately after treatments, and an overall improvement in her well-being. Due to the severity of her condition, permanent change in her spasming is unlikely, however a 20% reduction in spasms was observed during the course of treatments.
Subjective:
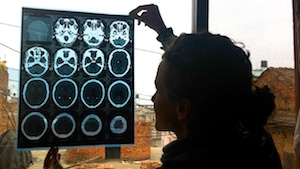
 38-year-old patient presents with involuntary spasming of her right and left hands, shoulders, head, feet and hips. Spasming started 4 years ago in her hands and feet exclusively. The spasming rapidly progressed to the rest of her body within a year and a half. When the condition started, she was taken to the hospital in Pokhara, Nepal where she received two CT scans and a panel of blood tests. The patient was then referred to a different hospital in Kathmandu where she began working with a neurologist. She was given an allopathic medication that made her sleep the majority of the day, only waking twice to eat. Over the course of 6 months, the patient visited the neurologist 3 times before discontinuing appointments. After those treatments, her family noticed that the spasming progressed to her head.
38-year-old patient presents with involuntary spasming of her right and left hands, shoulders, head, feet and hips. Spasming started 4 years ago in her hands and feet exclusively. The spasming rapidly progressed to the rest of her body within a year and a half. When the condition started, she was taken to the hospital in Pokhara, Nepal where she received two CT scans and a panel of blood tests. The patient was then referred to a different hospital in Kathmandu where she began working with a neurologist. She was given an allopathic medication that made her sleep the majority of the day, only waking twice to eat. Over the course of 6 months, the patient visited the neurologist 3 times before discontinuing appointments. After those treatments, her family noticed that the spasming progressed to her head.
At home, family members report that she becomes easily angered and frustrated, especially around her delayed speech. She also experiences poor memory, concentration, and is unable to handle tasks around the home. Patient expresses feelings of depression and anxiety around her worsening condition. She reports poor sleep due to the involuntary movement. Lastly, she complains of her skin being dry and itchy on her legs, arms, back and chest.
Other than the involuntary spasming and body itching, she does not have any significant symptoms as evaluated by a thorough review of systems.
The patient does not have any medical records available. Her understanding of her condition is limited to “a neurological problem.” Her mother and sister also experience the same condition in varying severities.
Objective:
Patient presents with bilateral, rapidly spasming movements of her hands, shoulders, head, feet and legs. While she is standing, the right side of her body swings from posterior to anterior. Her hips pop forward causing her back to arch. Her head moves in a fluid, circular motion towards the left. Left hand fingers have a rapid flexion and extension of the third, fourth, and fifth fingers. The thumb contracts over each of those fingers approximately 62 times per minute. The left hand is noticeably worse than the right. The patient’s right foot spasms from medial to lateral at a rate of 18 spasms per minute and with a delay of 1 to 2 seconds between spasms. While in the prone position, her right shoulder contracts backwards roughly 34 times per minute. When a response is required from the patient, her speech is delayed for 3 to 5 seconds, appearing difficult for her to formulate sentences. It is common for her responses to be short and minimal, and often times questions are not answered correctly compared to the answers given by her sister-in-law. When asked about the onset of her condition and any other related questions requiring a chronological sequencing of events, there seems to be confusion and lack of accuracy in her responses.
When asked to focus on controlling the spasms in her left hand, it is observed that they become worse in amplitude and frequency. Patient’s eyes are unfocused and often diverted to the right. She has some difficulty making eye contact while in conversation. Eye tracking test is done and shows an inability to follow the finger without movement of her head. The majority of the skin on her body is dry and has raised eczema-like bumps.
The tongue is pale, scalloped on both sides, cracks running horizontally in the centre, and is wet.
Assessment:
DX: Central Nervous System Degenerative Disorder
Due to the lack of medical records, it is important that there be a general discussion of possible neurological conditions that the patient may have in order to distinguish a potential diagnosis. Because her condition might potentially be in the earlier stages, diseases such as amyotrophic lateral sclerosis, Parkinson's, multiple sclerosis and Huntington's must be considered.
It is unlikely that the patient has Parkinson's disease. Parkinson's patients have slow and stiff body movements, rigidity of muscles, impaired balance, often a stooped posture and gait shuffle. Parkinson's patients may also experience non-motor symptoms before full-onset including drooling, change in taste/smell, choking and swallowing difficulties and cognitive impairment (Parkinson's Society of Canada). The patient has not reported any of the aforementioned non-motor signs when her condition began 4 years prior.
Amyotrophic Lateral Sclerosis (ALS) is also unlikely. Patients with ALS often present with signs and symptoms that are common in a wide variety of other neurological disorders, especially in the early stages. However, similar to Parkinson's, the presentation generally includes tightness, stiffness, weakness and muscular cramping. This patient presents with more choreal (spastic) movements than typically seen in an ALS or Parkinson’s patient.
This patient could be experiencing a form of Multiple Sclerosis (MS) called Primary-Progressive MS (PPMS). PPMS is characterized by a steady worsening of neurologic functioning without any distinct relapses or periods of remission (nationalmssociety.org). The patient’s symptoms, primarily the spasming, started 4 years ago and has gradually worsened to the extent at which they are now. Other common signs of MS include urinary incontinence, constipation, extreme fatigue, pain, numbness and tingling. Because the criteria for properly diagnosing MS is so broad, and the degrees of symptoms vary, it is difficult to rule out with proper imaging. However, it appears that MS is a less likely diagnosis because the patient does not experience some of the more common signs such as extreme fatigue and pain-associated symptoms.
Huntington's Disease (HD) is the strongest candidate for a diagnosis. It is important to note that in early stages of HD, there are subtle signs of physical deterioration, such as involuntary movements beginning in the hands and feet, difficulty in walking, and an increase in difficulty performing daily activities (ie. household chores). The patient reports that the spasming started in her hands and feet, and over time, gradually moved up to her head and shoulders. Her family has reported changes over time in her cognitive abilities to recall information, and confusion when it comes to organizing routine matters. The patient also reports substantial feelings of depression and anxiety, which are consistent with an HD presentation. The most compelling evidence for a HD diagnosis would be the chorealike movements. Unlike the jerky, rhythmic movements of ALS or Parkinson's, Huntington's patients experience uncontrollable, fluid movements, often with a puppet-like gait. This is consistent with the patient’s presentation.
Further neurological testing would need to be done for a complete and accurate diagnosis.
TCM DX: External attack of wind on the channels and collaterals
Due to the fact that other than the obvious tremors, there are no signs of an underlying organ pathology, either excess or deficiency, the source of the wind must be external.
Prognosis:
Poor. Due to the onset of this condition in middle age, it is unlikely that the patient will experience full reduction of the spasming. In fact, if a diagnosis of Huntington’s Disease is correct, it is expected that the condition will progress in spite of treatment. The goal of treating the patient is to aid in overall well-being, potentially slowing the progress of the degeneration of the central nervous system, and subduing the spasming. This can be accomplished through the use of acupuncture, Chinese herbs and patient counseling. Focusing on memory and speech improvement will give the patient a greater sense of independence. Referral to an appropriate hospital that will be able to provide a complete neurological examination will further the prognosis and outcome of this case..
Initial plan:
Due to the severity of the patients condition, daily acupuncture treatments are prescribed. Fortunately, the patient lives 15 minutes away from the clinic, and is able to walk unassisted to the clinic for treatment.
Overall, initial focus is to expel wind in the whole body to reduce the spasming, while simultaneously nourishing constitutional blood and qi. Typical acupuncture treatment includes combinations of SP10, SP6, ST36, LR8, LR3, RN4, RN6, LI4, DU19, GB 20.
Patient is counseled on the prognosis of her condition, the unlikelihood of a total reduction in the spasming, as well as the positive effects that acupuncture can have on her overall well-being and daily life.
The patients signature and drawings of circles and squares are recorded before and after acupuncture treatments to measure if there is a reduction, or stabilization, in her movements.
Outcome:
After 3 treatments, it appeared that when direct attention was focused on her during needling, her movements became more dramatic and active. A different approach was taken by placing her prone, and using the the Hua Tou Jia Ji (HTJJ) points to help sedate her during treatment. In addition to HTJJ, the back (shu) transporting points of the Heart, Pericardium, Liver, Blood, Spleen, Stomach and Kidney were needled to tonify those organ’s qi and to nourish blood.
After a period of treatments, patient reported that she experienced a feeling of 'lightness' during and after treatments. While the needles were retained, there was a significant difference observed in the amplitude of spasming and movement. The movements appeared to be smaller and smoother, and there was a general calmness about her body (see video # 2). There was less of a delay before she would start to speak. She sounded more clear and less interrupted. She was sleeping better at night and waking less frequently. The patient was asked to draw circles and spirals before and after treatment. There was a noticeable difference in the after-treatment drawing. It appeared that her hand was able to steady the pen and press more firmly on the paper (see visual). The drawing process was done every 2 or 3 treatments. She requested that this be done every time, and seemed to look forward to seeing if there had been progress made. Over the course of 13 treatments, her overall demeanor had improved. She came to the clinic with a smile on her face, and each time, more fully engaged in conversation with the practitioner. Family reported that after a period of time, they noticed that she was less frustrated in her speech, and in performing tasks around the home.
Please see links below for recorded evidence of the before-and-after, with needles retained for roughly 15 minutes.
Conclusion:
The challenge in this case was the lack of allopathic diagnosis and medical records, coupled with the rapid progression of the patient’s condition over the last 4 years. However, it was clear that a significant difference was made in her life through the use of acupuncture and the building of a therapeutic relationship. The need for education about her condition could not be stressed enough in helping her understand and prepare for the potential of it worsening in severity. Family education is also important, at least in part for the purpose of patient support, so that they have an understanding of the severity and progression of her disease. In considering this patient’s case, perhaps the most important role for a practitioner would be to help the family research hospitals and neurological specialists and procedures that may be beneficial for the patient.