Jennifer Rankin RAc
November 2011
Overview
65-year-old female presents with dyspnea and continuous cough. The patient also presents with chronic, severe pain and inflammation of all joints of the hands and feet. With 9 acupuncture treatments and the use of Chinese herbs, the patient experienced a 6% O2 increase, more than a 50% reduction of pain and a 90% improvement in range-of-motion in her hands.
SUBJECTIVE
65-year-old female patient presents with chronic dyspnea and continuous cough. The difficult breathing started 4-5 years ago and has become progressively worse. The patient does not live in a high traffic area, but has used an indoor fire to cook for most of her life. She now uses gas. The difficulty she experiences breathing is continuously present with no history of asthma attacks and no history of fever and chills. The patient does not report chest tightness or coughing at night. The dyspnea lessens with rest. Occasionally, cough is accompanied by small amounts of white or red phlegm. The dyspnea is the same with inhalation as with expiration. She reports not being able to walk from the microbus to the clinic (about 150 feet) without severe wheezing. It is hard to take a deep breath and she sometimes feels like she is unable to take in enough air. She also reports waking from difficulty breathing. The condition worsens in the winter, in the afternoon, and when walking or lifting. The patient has a family history of breathing difficulty including both her mother and sister who have had medical intervention concerning their conditions. The patient feels cold and gets common colds easily. She has spontaneous sweating.
The patient reports bilateral pain, inflammation and stiffness of all of the joints of the fingers and the feet including the ankles. The pain started 4 years ago while she was still working in the fields and has since gotten worse. Warmth helps the pain and movement makes it worse. The pain is burning, tingling and “unbearable.” There is no accompanying fever. The patient reports good energy and appetite. The pain is severe, worse in the afternoon, and interferes with walking and sitting. She has no family history of pain and inflammation in the joints.
The patient experiences pain in the shoulders and knees and a heavy, dull ache in the low back. The patient no longer does field work and does very little activity. No other medical treatment has been administered for these conditions.
Objective
 The patient has difficulty talking due to breathlessness and audible wheezing. When she moves, the wheezing increases. She has a weak and raspy voice with the occasional weak cough. She appears to be in average health for her age and environment. A strong wheeze can be heard through auscultation of her lungs. The first measurement on the oximeter is recorded at 91% O2. The patient is in moderate pain, indicated by her ability to smile, laugh and respond to questions. However, walking and sitting are difficult. All joints of the patient’s hands are swollen to 40% larger than normal and her feet and ankles are swollen to 30% larger. Both the hands and feet are hot to touch. No bone deformities are present. The patient has an 80% reduction in the active range-of-motion of all her finger joints and is unable to make a fist. She has a 30% reduction in the active range-of-motion of all the joints of her feet. The passive rangeof-motion of her joints was not tested.
The patient has difficulty talking due to breathlessness and audible wheezing. When she moves, the wheezing increases. She has a weak and raspy voice with the occasional weak cough. She appears to be in average health for her age and environment. A strong wheeze can be heard through auscultation of her lungs. The first measurement on the oximeter is recorded at 91% O2. The patient is in moderate pain, indicated by her ability to smile, laugh and respond to questions. However, walking and sitting are difficult. All joints of the patient’s hands are swollen to 40% larger than normal and her feet and ankles are swollen to 30% larger. Both the hands and feet are hot to touch. No bone deformities are present. The patient has an 80% reduction in the active range-of-motion of all her finger joints and is unable to make a fist. She has a 30% reduction in the active range-of-motion of all the joints of her feet. The passive rangeof-motion of her joints was not tested.
Pulses are deep, weak and soggy. Her tongue is pale and swollen.
Assessment
DX: COPD and osteoarthritis (pronounced in the joints of the hands, feet, knees and shoulder)
TCM DX: Lung and Kidney qi deficiency with wind-cold-damp bi syndrome in the joints
PROGNOSIS: Using acupuncture and herbal treatment, improvement is expected within 10 treatments. However, due to the severity of the pain, inflammation and breathing difficulty, more significant outcomes are expected over a longer course of treatment.
Initial Plan
Treat with acupuncture 3 times per week for 10 treatments before reassessing.
Focus on reducing swelling and inflammation (cold-damp bi) first. As swelling is reduced, add treatments to tonify the Lung (wei qi) and Kidney qi.
Typical points: LU1, REN17, LU9, KD3, SP6, LU5, ST36, LI4, UB 3, UB23, as well as local points at sites of swelling and pain
Du Huo Jie Xie Wan (8 TID) for first 2 weeks to reduce swelling and inflammation of the joints; Then switch to Ding Chuan Wan (8 TID) to tonify the Lung and Kidney qi
B complex vitamin with 100mg B1, 100mg B5 and 100mg B6 to assist with wound healing and as anti-inflammatory agent
Counsel the patient about proper ventilation of home if ever cooking with a wood fire and wearing a mask when in polluted or high traffic areas.
Outcome
After 9 treatments the patient reported major changes in her breathing, pain and inflammation. The patient’s voice was stronger with less audible wheezing and she could take a deep breath. She no longer had times when she felt like she couldn’t take in enough air. She wasn’t waking wheezing and she could walk from the microbus to the clinic with a very small amount of wheezing. The patient continued to have a regular cough, however it decreased from being continuous to 2-3 times per day. When phlegm was present it was only white. The pulse oximeter generally read between 95-97% O2 and only occasionally read 92- 93% O2.
The swelling in the patient’s hands completely resolved with only minor swelling of the lateral ankles. The hands were no longer hot to touch and the patient reported no feelings of heat in the joints. The pain decreased over 50%. The patient had full active and passive range-of-motion in her feet and had a 90% increase in the active range-of-motion in her hands. She was able to walk and sit without severe pain and make a complete fist.
Continued Treatment
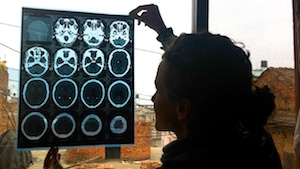
This patient needs continuous, intensive acupuncture and herbal treatment for her lungs and arthritis. Continued monitoring of oxygens saturation rates, lung auscultation and a chest x-ray are objective measures of her progress that would be beneficial. The patient has responded positively to treatment thus far and further improvement is expected.
Conclusion
The effectiveness of acupuncture and herbal medicine for both COPD and arthritic pathologies is clearly outlined here. The importance of regular treatment and the use of objective measures to quantify progress is essential.