Marlena Pecora MSAOM, EAMP, LAc
December 2013
Overview
70-year-old female presents with acute abdominal, chest and scapular pain, vomiting and diarrhea. At the local hospital, she was diagnosed with acute cholecystitis via labs and ultrasound. She received anti-nausea medication and was turned away for further treatment. After 7 treatments using acupuncture and Chinese herbal medicine, the patient’s pain improved 90%, and she had complete resolution of vomiting, nausea and diarrhea.
Subjective
Patient presents with severe abdominal chest and scapular pain. Onset occurred 2 weeks prior with an increase in severity 4 days ago. The pain in the abdomen is achy, and at times sharp in the upper right quadrant, and radiates across the abdomen. The chest pain presents behind the sternum, and radiates to the scapular region. Pain is worse with deep inhalation, and affects her daily activities. Patient reports whole body pain and feeling feverish. Her body feels heavy and she lacks appetite. She experienced nausea and 6 bouts of vomiting in the last 2 days. Her stools have been loose, and darker in color for the last 2 days. 10 days prior to her visit to the clinic, she had been evaluated and treated at the local hospital for the same severe pain, nausea and vomiting. She reports being diagnosed with gallstones, and treated with anti-nausea and asthma medication. The patient reports being told she was too old for surgery. Prior to the acute symptoms, she had been eating a diet of rice, lentils, vegetables and meat, a diet high in oils and fats.
Objective
The patient appears physically uncomfortable and distressed. She has a dull gray pallor, orbital edema, red eyes, and a flat affect. Sitting slouched in the chair, her responses are short and eye contact is minimal. Her breathing is labored and slightly rapid. Patient displayed involuntary guarding of the upper abdomen. There is severe pain upon mild palpation of the upper right and left quadrants of the abdomen. Murphy's sign is positive upon first visit (deep inspiration exacerbating pain during palpation of the upper right quadrant halting inspiration). The back pain is moderate upon moderate palpation around the scapula region. Vital signs at first visit were slightly elevated. Blood pressure is 150/95 mmHg, pulse rate 115 beats per minute, respiratory rate of 27 breaths per minute, temperature 99.5 degrees Fahrenheit and 93 spO2.
Patient's tongue is very pale, and puffy with grey scalloped edges, especially on the right side with a thick greasy yellow coat. Her pulse was rapid, and slippery.
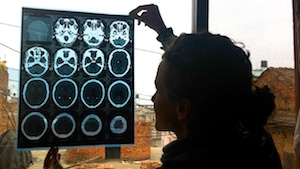
The patient brought in medical records from her prior visit to the local Hospital. Labs revealed elevated serum bilirubin total and direct, and serum amylase levels. An ultrasound (USG) of the abdomen revealed a calculus of 13mm in the gallbladder lumen.
Assessment
DX: Acute cholecystitis
TCM DX: Damp-heat in the Liver and Gallbladder; Underlying SP qi deficiency with damp accumulation; LU qi deficiency
Prognosis
Acute cholecystitis usually subsides within 2 to 3 days, and resolves within 1 week in 85% of patients. Due to the patient’s age and lack of resources and history of asthma, a routine choleosystecomy was not performed during her hospital visit. Complications of acute cholecystitis include an infected gallbladder progressing to gangrene, or perforation of the gallbladder if left untreated. The patient is from a small village that lacks healthcare. She travels 2 hours each way to the clinic. With proper monitoring of the patient’s condition, acupuncture and Chinese herbal medicine treatments, the patient’s severe pain and acute symptoms will likely resolve within 6 treatments.
Initial plan
Patient is to be treated at clinic 3 times per week for 3 weeks. Monitoring of patient’s vital signs and symptoms to be assessed at each visit. Focus on reducing pain, inflammation of gallbladder, and preventing further complications. Acupuncture and Chinese herbal medicine, with focus on draining damp-heat from foot Shaoyang channel, and moving qi and blood. If symptoms do not reduce at each treatment, or vital signs worsen, patient will be referred to the hospital for complications of acute cholecystitis. Nutritional education to be incorporated into treatment.
Typical Treatment
Acupuncture: Dannagxue, right GB34 and right GB40 with electroacupuncture 5Hz continuous; LV2, UB19, UB18, UB20, ST40, LV14, GB44, GB40, GB21, REN10, REN12, Ling Gu, Da Bai and left auricular LV/GB point.
Cupping: Stationary cupping along Bladder channel from cervical to mid-thoracic region x 8 bilateral.
Chinese herbs: The patient is treated with Chinese Herbal Medicine. At the first visit, she is given Da Chai Hu Tang, 8 tea pills TID for 14 days. Ban Xia Xie Xin Tang is added at the fourth visit, 3 capsules TID for 12 days.
Lifestyle advice: Nutritional recommendations of a low fat, high fiber diet are discussed. Patient is advised to incorporate more turmeric and mint tea into diet. In Chinese herbal medicine, turmeric rhizomeis known as Jiang Huang. It invigorates the blood, reduces blood stasis, reduces pain, and drives qi downward. Pharmacologically, turmeric acts as an anti-inflammatory, anti-hyperlipidemia, antibacterial and hepatoprotectant agent. It is easily accessible in the region of Nepal in which the patient lives. Mint is to help reduce pain with its natural anti-spasmodic effects, and grows abundantly in the region.
Outcome
The patient showed progressive improvement throughout all 7 treatments. At treatment 7, the patient experienced a total of 90% reduction in abdominal and scapula pain, with complete resolution of chest pain. Patient reported her digestion as good, with no gas or bloating, and a complete resolution of nausea, vomiting and diarrhea. Patient’s affect was brighter, she was talkative, smiling and made full eye contact. Her tongue appeared less puffy and greasy, and her pulse less rapid. All vital signs were improved, blood pressure 140/95 mmHg, pulse rate 95bpm, respiratory rate 22 bpm, and 95 spO2.
Conclusion
This case was significant because of the severe pain with which the patient presented, and her lack of options. The patient received 7 acupuncture and Chinese herbal medicine treatments in 2 and a half weeks. She experienced 90% reduction in pain with complete resolution of diarrhea, nausea and vomiting. Due to the patient’s age, economic standing and past medical history, she was unable to have a cholecystectomy. She received anti-nausea and asthma medication, and was turned away for further treatment at the hospital. Acupuncture and Chinese herbal medicine helped to reduce her pain, systemic symptoms, and improve her overall quality of life.
Chronic cholecystitis, long standing gallbladder inflammation commonly due to gallstones, is a potential future complication. To help prevent future complications, management of the gallstones themselves is necessary. A modified diet of less fats and oils and more vegetables is recommended. Continued treatments with acupuncture and Chinese herbal medicine is also recommended. The gallstone, and gallbladder function, should be reevaluated by ultrasound and labs to monitor progress.